Yellow fever is a viral disease caused by the yellow fever virus. The disease was first identified in 17th-century Europe, and it has since spread to Africa, Asia, North America, South America, and Oceania.
The walter reed yellow fever experiment is a historical event that occurred in 1901. It was conducted by Walter Reed to test the effectiveness of the vaccine for yellow fever.
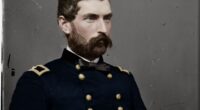
Walter Reed, a U.S. Army doctor, helped the world overcome yellow fever and earned a place in history.
The two 14-by-20-foot experimental shacks stood 80 yards apart on a broad, grassy plain at Camp Lazear, near Quemados, Cuba, under the supervision of US Army Major Walter Reed, MD. On each side, clusters of white canvas wall tents stood at a respectable distance, as though hospital visitors were hesitant to approach the terminally sick.
The shacks seemed unremarkable from the outside. Their custom-designed interiors, on the other hand, were everything but. Visitors had to walk through small vestibules to access the interior rooms, which were securely sealed and equipped with screened double doors. Three beds and “three big crates packed with linens, pillowslips, blankets, etc., contaminated by contact” with sick people were kept in Building No. 1, which was heated to 95 degrees Fahrenheit.
On December 5, 1900, medical history was created in Building No. 2, which was separated in two by a fine-mesh wire screen. Private John R. Kissinger entered one side at 2:30 p.m., relaxed on the sole bed, and allowed himself to be repeatedly bitten by five ravenous mosquitoes, each afflicted with the deadly yellow disease.

The final two decades of the 1800s saw an incredible flurry of medical breakthroughs. Brigadier General George Miller Sternberg, a physician of the United States Army, discovered the bacteria that causes pneumonia in 1881, while Louis Pasteur, a French microbiologist and chemist, developed an anthrax vaccine the same year. Antitoxins were found in 1890, and Theobald Smith, an epidemiologist and pathologist who worked for the US Department of Agriculture’s Bureau of Animal Industry, was the first to prove that ticks transmit Texas cow disease in 1892. But it was Reed, one of the world’s finest medical researchers, who produced the most important breakthrough in the century’s last month. It was a watershed moment in the fight against yellow fever, a disease that had claimed the lives of 100,000 Americans during the preceding century. Yellow fever had devastated port towns like New Orleans and Philadelphia after being imported from the tropics, killing 40 percent or more of those afflicted.
Walter Reed was born in Belroi, Virginia, on September 13, 1851, the son of a circuit-riding Methodist preacher. He started exhibiting some of the qualities for which he would later be recognized while he was still a child: self-control, a strong sense of dignity, and an unquenchable desire for information. Reed’s early education was irregular, but his family relocated to Charlottesville, Virginia, in 1866, and he enrolled at the Charlottesville Institute, a one-building institution that prepared him for his next scholastic experience.
Reed enrolled at the neighboring University of Virginia when he was 16 years old, in 1867. Because of his age, he needed special permission. Reed studied Latin, Greek, and English literature, among other courses, that year, according to one of his instructors.

Reed intended to attend Mr. Jefferson’s university for the entire course, but due to the fact that two of his brothers were already enrolled and his family’s financial resources were limited, he decided after his first year to ask the faculty for a bachelor’s degree in the subjects he had already studied. However, since he was so young, his request was denied.
Reed then asked in a faculty meeting whether he might be given the doctor of medicine degree, which at the time required a two-year course of study, provided he passed the required exams the following year. Several academics agreed that this was an absolute impossibility.
“Doctor,” Reed allegedly remarked to Socrates Maupin, a 60-year-old chemistry professor and faculty chairman, “you have heard these gentlemen.” Will you check to verify whether I have my MD degree if I meet the minimum requirements?” When Maupin said he would, Reed bowed to the other faculty members and said, “Gentlemen, I hold you to your word,” before exiting the room.
Reed immersed himself into his studies, taking chemistry, medicine (including legal medicine and obstetrics), physiology and surgery, anatomy, and materia medica (pharmacy). Maupin remarked that the 17-year-old student was the youngest ever to graduate from the University of Virginia Medical School when he gave Reed his diploma nine months later, in the summer of 1869.
Reed went from Charlottesville to New York City, where he received a second doctor of medical degree in 1870 from Bellevue Hospital Medical College. He completed his internship at different medical facilities around the city during the following five years. Reed was also named one of the five inspectors on the Brooklyn Board of Health in 1873, when he was 22 years old.

Reed met his future wife, Emilie Lawrence, in 1874 and chose to join the United States Army Medical Corps, which led to his world-changing study and the virtual elimination of yellow fever. Reed returned to his studies and, in February 1875, passed the arduous 30-hour test required to join the medical corps. Reed was commissioned as an assistant surgeon with the rank of first lieutenant the next year, and Lawrence was married the following year.
Years of boring garrison service preceded Reed’s successful army career. He served at Fort Lowell and Camp Apache in Arizona. Reed was in charge of not just the health of the military detachment and its numerous dependents, but also the health of the local Native American tribes. It was there that he first saw an epidemic—in this instance, smallpox—and the misery and death that accompanied it. Reed was sent to Fort McHenry in Baltimore in 1890, following postings in Nebraska and Alabama. He was given the position of attending surgeon and recruit examiner. Reed returned to the classroom at Johns Hopkins, the nation’s first research institution, where he studied pathology and the burgeoning discipline of bacteriology in a laboratory course taught by William Henry Welch, the nation’s finest pathologist. (Welch was one of the four founding professors of Johns Hopkins Hospital and the first dean of the Johns Hopkins School of Medicine, having trained under Louis Pasteur.) He was dubbed “the dean of American medicine” during his lifetime.)

Over the last ten years, our knowledge of infectious illnesses has vastly advanced. “There had followed in rapid succession,” Welch wrote, “such important discoveries as those of the specific germs causing anthrax, tuberculosis, leprosy, glanders,…tetanus, pneumonia, typhoid fever, malaria, amoebic dysentery, cerebro-spinal meningitis, diphtheria, and a large number of other diseases,” based on Pasteur’s early work on germ theory and new methods for
Reed was asked to go to the Washington, D.C., office of US Surgeon General George Sternberg, a renowned bacteriologist, in 1893 following another tour of service out west. Reed was named curator of the Army Medical Museum (later renamed the National Museum of Health and Medicine) and professor of bacteriology and clinical microscopy at the Army Medical School in Washington. Reed has also joined the Columbian University Medical School faculty (later the George Washington University School of Medicine).
Reed worked closely with Sternberg on a smallpox vaccine research while on these new duties, and in 1895, he witnessed a malaria epidemic near the nation’s capital. The next year, when yellow fever broke out among U.S. Army troops stationed near the Potomac River—enlisted men, but strangely, not their officers—Reed distinguished himself as a medical researcher. The troops, according to popular belief, got the disease after drinking river water. Reed demonstrated to local authorities that the epidemic was not caused by the dirty Potomac. Instead, he demonstrated how yellow fever was linked to the marshy forests that bordered the river: the ill troops were used to trekking through them at night while their commanders stayed in camp.
Reed’s experimental station was named after bacteriologist Jesse Lazear. (Alamy Stock Photos/Science History Images)
The United States declared war on Spain in April 1898. For the previous 30 years, Cuba had been roiled by revolts against Spanish authority. By the late 1890s, popular opinion in the United States supported Cuban revolt and independence, owing in part to allegations that concentration camps were being utilized to repress the Cuban people. On February 15, 1898, the armored cruiser USS Maine exploded and sunk in the port of Havana, Cuba, killing 260 men. American newspapers blamed Spain. On April 20, President William McKinley signed a bipartisan congressional resolution calling for Spain’s withdrawal from the island and authorizing US military involvement to assist the insurgents. Spain, on the other hand, was adamant on staying in Cuba. On April 24, it declared war on the United States, and the United States declared war on Spain a day later. The 10-week war in the Caribbean and Pacific, in which US naval strength proved victorious, resulted in Cuban independence and the sale of Guam, Puerto Rico, and the Philippines to the US for $20 million.
Despite the fact that the war was brief and relatively bloodless—only 332 Americans died in combat—the volunteer camps of the United States, both in Cuba and at home, were infamously disease-ridden. Almost 3,000 troops died as a result of the diseases that raced through the encampments like a reaper’s scythe. Spanish bullets were much less lethal than yellow fever and typhoid disease.
Following the conclusion of the combat in August, Sternberg appointed Reed to lead a board of officers tasked with examining the development of typhoid disease in the stateside camps. Reed traveled to training camps in Alabama, Florida, Georgia, Pennsylvania, Tennessee, and Virginia with Majors Edward O. Shakespeare and Victor C. Vaughan, both of whom had researched U.S. typhoid epidemics. They proved that typhoid is both infectious and contagious by analyzing each camp’s water supply, waste disposal, and food preparation and distribution, as well as tracking the disease’s spread. Because of inadequate cleanliness, it leaked into the water and subsequently spread among the troops. Infected bedding, for example, left behind by leaving troops, infected incoming soldiers who used it immediately. The illness was also spread by flies in the camps.
Reed’s “Typhoid Board” demonstrated that the illness was transmitted by flies, as well as people, drinking water, and items infected by fecal bacilli, in a huge two-volume study. The 46-year-old major was about to embark on his most significant contribution to medicine and humanity.
Reed was sent to Havana in May 1900 and assigned to the newly formed Yellow Fever Commission. His squad consisted of acting assistant surgeons from the United States Army. James Carroll, an Englishman with a medical degree from the University of Maryland, was in head of the bacteriology lab. Jesse Lazear, a bacteriologist who graduated from Columbia University College of Physicians and Surgeons’ medical school, was in charge of the laboratory work and eventually took over the care of the experimental mosquitoes. The pathology study was done by Cuban-American Aristides Agramonte y Simoni, a tropical medicine expert with a medical degree from Columbia University College of Physicians and Surgeons.

Many American troops stationed in Cuba were afflicted with the so-called “yellow plague” both during and after the war. According to Reed, the troops contracted yellow fever 1,575 times on the island, resulting in 231 fatalities. The feared “Yellow Jack” has also visited cities in the United States throughout the years. Between 1793 and 1900, the United States was hit by 95 yellow fever outbreaks, according to Reed. 500,000 Americans were afflicted and 100,000 died during that time period. With 41,348 fatalities, New Orleans was the “greatest sufferer,” according to Reed, followed by Philadelphia with 10,038 dead. In the 1850s and 1870s, four yellow fever outbreaks killed approximately 8,000 people in Memphis, Tennessee. A survivor of the city’s 1878 outbreak said, “There were hours, particularly at night, when the somber burden of universal death weighed upon the human soul, as if the day of judgment was about to dawn.”
This viral plague usually begins with a headache and abrupt chills, followed by severe bodily aches, vomiting, and a high temperature that may persist for weeks. Kidney failure and liver illness (which results in a sickly jaundice, thus the term) are also prevalent. These symptoms sometimes go away, signaling a potential recovery, but they typically return in full force, bringing with them internal bleeding and the dreadful black vomit that occurs when stomachs filled with blood are emptied.
When Reed and his colleagues arrived at Columbia Barracks in Quemados, Cuba, in June 1900, they set out to verify an Italian bacteriologist’s hypothesis that yellow fever was caused by Bacillus icteroides, a bacterium belonging to the hog-cholera group. When they couldn’t find a causal link, they decided to put the hunt for the particular agent on hold and focus on how it spread.
As a result, they went to Carlos J. Finlay, a Havana-based physician who graduated from Jefferson Medical College in Philadelphia. Finlay had maintained for 19 years that yellow fever was spread by the common house mosquito. “Not only its eggs, but also its salivary and venom glands may be invaded by pathogenous germs when the mosquito gets contaminated,” he wrote in 1881, “so that the latter may be discharged…when the insect attacks its next victim.” The medical world laughed at him as “the mosquito guy,” the crazy Cuban who believed that insects might transmit yellow fever since he was so far ahead of his time and his theory hadn’t been proven under laboratory settings.
Reed’s team decided to put Finlay’s theory to the test using an unconventional method: real people. “The Commission concluded that the results, if positive, would be sufficient service to humanity to justify the procedure, provided, of course, that each individual…was fully informed of the risks he ran, and gave his free consent,” wrote Howard Atwood Kelly, another of Johns Hopkins Hospital’s founding professors. Two dozen individuals courageously volunteered for this possibly deadly experiment, including troops from neighboring Columbia Barracks and a few Spanish immigrants.
The commission members, on the other hand, agreed that it was their responsibility to be subjected first.
Private John R. Kissinger volunteered for Reed’s experiment and became the first person to get yellow fever under controlled conditions. (University of Virginia’s Claude Moore Health Sciences Library)
According to Carroll, numerous insects were “reared in the laboratory” using Finlay’s small black mosquito eggs and “made to feed upon four instances of yellow fever, two of them serious.” Carroll and Lazear bravely agreed to get bitten by the contaminated insects, and both men contracted the illness shortly after. Carroll subsequently stated, “Thus it occurred that I was the first person to whom the mosquito was shown to transmit the illness.” “After many days of insanity and black vomit, Dr. Lazear was struck and died in convulsions only one week later.”
Despite being saddened by the death of one of his physicians, Reed was pleased to present the team’s findings to the Public Health Association on October 23, 1900 in Indianapolis. “The mosquito serves as an intermediary host for the yellow fever parasite,” Reed said to the crowd.
More experiments—tests conducted under tight laboratory control—were needed to establish this clearly to the public, as well as to disprove the notion that the illness was spread through dirty clothes. “Some method must be given by which complete control could be exercised over the movements of the people exposed to experiment for some time previous to inoculation, in order to eliminate every potential source of infection save the mosquito,” Kelly wrote.
Camp Lazear, a strictly confined experimental station named for the brave doctor, was created one mile from Quemados on November 20, 1900, and the two experimental shacks were built. Three volunteers spent 20 nights in Building No. 1, dubbed the “Infected Clothing Building,” covered in filthy bedclothing. Private Kissinger permitted himself to be bitten repeatedly by infected mosquitoes in Building No. 2—the “Infected Mosquito Building.” He produced what is thought to be the first case of controlled experimental yellow fever within days. (Kissinger healed and returned to Indiana, only to be paralyzed in his legs for 13 years as a result of his yellow fever infection.) Congress gave him a $125-per-month stipend, friends bought him a house, and he was given the Medal of Honor in 1929. In 1946, Kissinger passed away.)
In the weeks that followed, 20 additional instances of the terrible disease were discovered. Finlay’s previously criticized hypothesis was validated by these findings. Yellow fever was not acquired by any of the volunteers who stayed in the Infected Clothing Building. Exposure to tainted textiles presented no risk at all, which was a surprise finding given long-held common perception. According to historian Philip Alexander Bruce, these discoveries constituted “a watershed moment in the history of preventative medicine.”
In a letter to his wife, Reed wrote, “It is with great joy that I hurry to inform you that we have succeeded in generating a case of unmistakable yellow fever by the bite of the mosquito.” “Rejoice with me, darling, since it will be considered as the most significant piece of scientific work throughout the nineteenth century, apart from the antitoxin of diphtheria and [Robert] Koch’s discovery of the tubercle bacillus [the bacteria that causes tuberculosis].”
As Bruce phrased it, Reed’s finding would one day open “a new chapter in the history of huge tropic areas.” Yellow fever was eventually eradicated from the island of Cuba by eliminating mosquito breeding grounds. Similarly, the Panama Canal Zone was eventually free of the death-dealing insect’s ravages.
Reed received much praise for his efforts in the scientific community. He was now on par with Crawford Long, the discoverer of anesthetics, Joseph Lister, the inventor of antiseptics, and Edward Jenner, dubbed “the Father of Immunology” for pioneering the idea of vaccination.
Reed returned to Washington in February 1901 and resumed his teaching duties. At the Army Medical School and Columbian University Medical School, he taught pathology and bacteriology. “He was a popular with his pupils because he communicated a passion for his topic that is the characteristic of outstanding teachers,” said historian Ralph Nading Hill.
Reed received two honorary degrees in the summer of 1902: a doctor of law from the University of Michigan and a master of arts from Harvard University. Reed was appointed librarian of the surgeon general’s library the following November. “Mental effort, on the other hand, was becoming curiously unpleasant to the alert mind that had usually approached it so buoyantly,” observed biographer L. N. Wood. He persisted in pushing himself until, unable to hide his diminishing strength from his wife, he sought medical advice. It was already beyond the point of no return. Appendicitis was detected on November 13 by doctors. He had his appendix removed, but peritonitis had already set in. On November 23, 1902, Reed died and was interred at Arlington National Cemetery. He was just 51 years old when he died.
New Orleans—the American city that had lost the most people to Yellow Jack—suffered just one more outbreak in 1905 after implementing the mosquito-elimination methods suggested by Walter Reed’s Yellow Fever Commission. It was the final yellow fever epidemic in the United States.
Walter Reed General Hospital, which was established in 1909 on 113 acres in the District of Columbia and is named after him, served as the U.S. Army’s top medical institution for more than a century. It served over 150,000 current and retired military members throughout its tenure on the front lines of medical duty. The army dedicated Walter Reed National Military Medical Center, a large hospital complex, on the grounds of the National Naval Medical Center in Bethesda, Maryland, in 2011. Its successor, Walter Reed Army Medical Center, functioned from 1977 to 2011.
Mrs. Reed remarked after her husband’s death, “When his great task was over, the pleasure which filled his spirit was completely for the pain he would save mankind.” He was overjoyed that his life had not been in vain, and that God had seen fit to use him for good.” MHQ
Rick Britton is a Charlottesville, Virginia-based historian and cartographer.
The what is walter reed known for is the Walter Reed Army Medical Center. It was founded in 1879 and has been a major player in the military health care system ever since.
Frequently Asked Questions
Who Solved yellow fever?
The answer is yellow fever was solved by the Yellow Fever Vaccine Initiative.
What disease did Walter Reed investigate during the Spanish American War?
Walter Reed was a doctor who investigated diseases during the Spanish American War.
Which doctor first developed a mosquito hypothesis?
The first doctor to develop a mosquito hypothesis was Dr. William Farr in 1876.
Related Tags
- interesting facts about walter reed
- how did walter reed discovered yellow fever
- who was walter reed and what did he do
- walter reed typhoid fever
- walter reed malaria research